Need help now?
If you or someone you know is experiencing an emergency, please call 911. If you think it would be beneficial to have a mental health professional assess and connect the person with services, tell the dispatcher that you’d like to request the Mental Health Response Team (MHRT).
If a team member is not available, a patrol officer will respond to assist. All Fort Collins officers receive training related to mental health response. If you'd like follow up from the MHRT, just let the responding officer know and a member of the team will contact you at a later time.
Use this flow chart to answer a few basic questions and determine the best local resource for your situation.
Mental Health Response Team#

Program Vision: We believe healthy communities are safe communities, that mental illness is not a crime, and that jails/hospitals should not be seen as the best ways to access appropriate care leading to long-term wellness.
Program Mission: To provide professional, compassionate, and comprehensive services through police/mental health collaboration through on-scene assessment and follow up aligned with the agency's de-escalation philosophy.
Program Goals: Increase on-scene safety for all involved parties. Route citizens to the most appropriate level of care. Avoid unnecessary referrals to hospital emergency rooms. Reduce incarceration related to crimes secondary to mental illness. Provide follow up care coordination to ensure citizens are able to access appropriate care. Create a culture of police-mental health collaboration with a focus on community need and collaboration.
Community Resources#
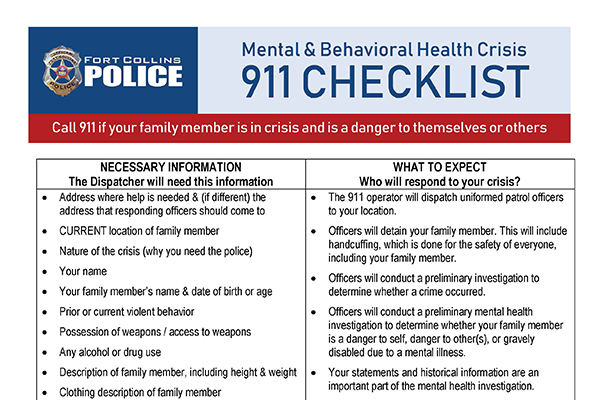
911 Checklist
Please call 9-1-1 if you or someone you know is in danger of self-harm or hurting others. This checklist will help you prepare and know what to expect when you call for help in a mental health crisis situation.
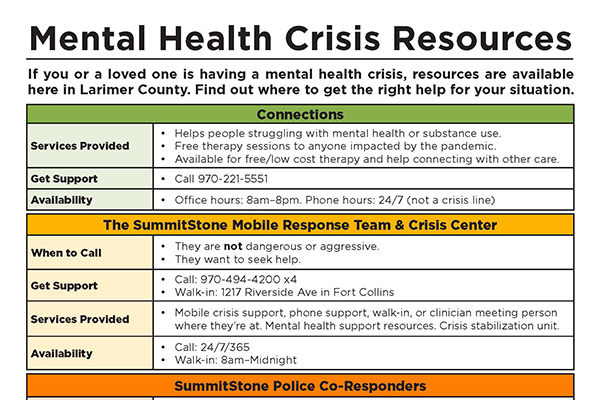
Larimer Resource Guide
If you or a loved one is having a mental health crisis, resources are available here in Larimer County. Click to view a list of local services.
Navigating a Mental Health Crisis
The National Alliance on Mental Illness (NAMI) created this guide to help people experiencing a mental health emergency.

Dementia Resources
Access local resources for those living with dementia, as well as support information for their caregivers and loved ones.
Medication Assisted Treatment
The Colorado Opioid Synergy for Larimer and Weld (CO-SLAW) counties is a network of clinics that offer medication assisted treatment and counseling services.
Mental Health Co-Responder Program History#

FCPS assists an increasing number of community members with behavioral health conditions, as well as their families who are concerned about them, on a daily basis. The Mental Health Co-Responder Program was created with the goals of 1) helping families and individuals in crisis access appropriate community services, and 2) increasing the safety of those individuals and officers who encounter them.
This program is an integral part of the agency's overall philosophy of de-escalation, or in other words, aligned with the philosophy of connecting with and helping community members without the use of force as often as possible.
Program Phase 1
Fort Collins Police Services began working to develop a co-responder program in 2015, and the program officially launched in July of 2018. Licensed professional counselor and addiction counselor Stephanie Booco was initially hired to serve as a full-time co-responder clinician. This position was jointly funded through FCPS, UCHealth, and SummitStone Health Partners.
Program Phase 2
In 2019, UCHealth Community Paramedic Julie Bower joined the program and Booco’s position fully transitioned to UCHealth in order to help facilitate the regional expansion of law enforcement co-response partnerships.
Program Phase 3
In 2020, FCPS approved the formation of a full-time Mental Health Response Team. In January 2021, two officers began working with the clinician and community paramedic to enhance mental health services to our community members and expand partnerships with local service providers. In 2022, the unit expanded to three officer-clinician teams and added a sergeant to support MHRT efforts.
* Internship opportunities are not available at this time.
-
Mental health has long been a topic of discussion, but it only recently became a focal topic of broader social interest. There are often questions about resources and why we do what we do. Below is some background on how we got to our present model.
1960s
Legislation was passed to deinstitutionalize psychiatric facilities, or in other words, the government wanted to find a way to better meet the needs of individuals with a mental health condition that allowed them to remain in the community. This piece of legislation, coupled with the Community Mental Health Construction Act of 1963, created significant changes in where and how people accessed mental health services, as well as what services were available. In effect, it closed inpatient facilities and encouraged states to open community mental health centers (CMHC) – treatment agencies where people with a mental health condition could go for medication and treatment while living in the community as opposed to residing in an inpatient facility. Additional court cases (see Lake v. Cameron, DC Court of Appeals, 1966) supported the idea of community mental health and treatment in what we refer to in the clinical field as the “least restrictive treatment setting” possible.1970-1980
In the 70s and 80s we saw court cases and legislation such as the 1975 US Supreme Court ruling in O’Connor v. Donaldson that changed the way we look at mental health holds and involuntary treatment. In this case, the courts ruled that a person must be a danger to self or others in order to be “constitutionally confined,” or otherwise known as being placed on a mental health hold and further assessed until stabilized. Years later, we see the Omnibus Budget Reconciliation Act pass that terminated federal government funding for mental health hospitals and required a medical illness for admittance to facilities. This required states to return to funding non-nursing homes for the long-term care of people in the community with severe and persistent mental illness (SPMI), which resulted in the segregation of this group into large, underfunded facilities. These facilities were often for-profit and privately owned, creating incentive for reduced costs to increase profits.1990s
Finally, the U.S. Supreme Court in Olmstead v. L.C. (1999) ruled that mental illness is a disability and covered under the Americans with Disability Act (ADA). This required all government agencies to move people with mental illness into community-based treatment settings again to decrease/avoid institutionalization.Impacts
With these legislative changes and landmark court cases, the actual practice of mental health care has experienced myriad expected and unexpected consequences. A reliance on insurance to cover treatment has increased, individuals with SPMI and more often living in the community and accessing resources at local healthcare centers which has proven excellent for social connection and health for most, but there is still a subset of this group that needs more support. These individuals are in contact with public safety partners, such as police, fire, or emergency medical services. When in contact, they are at different points of understanding the condition they are diagnosed with and motivation to address it in a way that is aligned with their best interests.To this end, public safety personnel, especially officers, are interacting with these individuals more often and thus one of the unintended consequences is an over reliance on public safety to provide the same level and quality of mental health assessments, treatment, and triage that a highly trained mental health professional would provide. We are beginning to see the other side of the system slowly catch up to the circumstances created by years of well-intentioned change that led to disproportionate rates of homelessness, incarceration, and compounded medical and mental health care problems for individuals in this group.
Present Day
In 2013, Senate bill 17-207 was passed. It was intended to end the use of the criminal justice system as a “holding space” for individuals with a mental illness. The legislation declared a behavioral health crisis to be a healthcare issue, not a police or criminal issue, and led to the creation of a “coordinated behavioral health crisis response system.” Governor Hickenlooper followed this up in 2016 with the Colorado Community Paramedic Bill, which allows community paramedics to practice emergency medical procedures during calls for service.Enter co-response and mobile integrated healthcare. Some areas had already recognized a need for these programs back in the 1980s/1990s and started putting these programs in place. Los Angeles Police Department and the CAHOOTS program in Eugene, Oregon are two examples of this. Today, there are national training sites for co-response (a mental health provider and officer working together) and mobile integrated healthcare (MIH) programs (a multidisciplinary team that responds to both in-progress calls for service and provides intensive follow up).
Behind the Scenes#
Episode 1: Meet MHRT
Go behind the scenes with members of the Mental Health Response Team. In this podcast-style discussion, an officer and clinician share their day-to-day work, the challenges they face, and what motivates them to serve. [31:35]
Note: Officer Annie Hill was promoted to sergeant shortly after this recording. While no longer a member of MHRT, she continues to support our community members in crisis as a Patrol shift supervisor.
Dallas' Story
Every day is an opportunity to travel a new path, and every person we encounter deserves to be treated with dignity at all stages of their journey. Listen to Dallas share his inspiring story of working through trauma and decades of addiction to find recovery with the support of local people who believed in him. [24:30]
[tw: full episode includes candid discussions about trauma, substance use, and self-harm]
Interagency Treatment Group#
The Interagency Treatment Group is a monthly forum of 25 community agencies; medical, mental health, social service, criminal justice and law enforcement, designed to assist Fort Collins Police Services in its efforts to intervene safely and effectively with individuals who exhibit mental illness and addictive behaviors.
Law enforcement, fire, mental health, medical, justice system, and community social service agencies interact with many of the same individuals with mental illness or dual diagnosis issues on a regular basis. The best use of limited community resources requires effective coordination of services. The Mental Health Co-Responder attends this meeting to facilitate coordination of intervention efforts.
The program’s mission is to bring together agencies that share clients with law enforcement in order to effectively coordinate services between agencies, provide the most effective interventions, reduce recidivism, enhance the safety of all service providers, and provide education and emotional support for agency representatives.
Mental Health Response Team Staff#

Sierra Black, LCSW
UCHealth Behavioral Health Clinical Co-Responder | noco.coresponse@uchealth.org
Sierra joined the Mental Health Response Team in June of 2022. She received both her Bachelor's and Master's Degrees in Social Work from Colorado State University and is currently a Licensed Clinical Social Worker (LCSW). Sierra has spent her career serving the community of Northern Colorado in various roles including victim advocacy, case management, inpatient care, mobile crisis response, and co-response.

Officer Chris Bland
MHRT Officer | mhrt@fcgov.com
Officer Chris Bland began his career with Douglas County Sheriff’s Office in 2013 and FCPS in 2019. Chris has bachelor’s degrees in sociology/criminal justice and political science, extensive experience working with individuals in crisis, and is a certified Crisis Intervention Teams (CIT) instructor. CIT is a nationally recognized model designed to help people with mental and/or substance use disorders access medical treatment rather than place them in the criminal justice system. Through collaborative community partnerships and intensive training, CIT improves communication, identifies mental health resources for those in crisis and ensures officer and community safety.

Brenna Rush, LCSW
UCHealth Behavioral Health Clinical Co-Responder | noco.coresponse@uchealth.org
Brenna Rush joined the Mental Health Response Team in January 2024. She received a Bachelor's of Psychology and a Masters in Social Work at Colorado State University. She is a Licensed Clinical Social Worker and a Licensed Addiction Counselor. Brenna has served the Fort Collins community for over 10 years with experience working in corrections, substance abuse treatment, outpatient therapy, and housing. Her specialties include severe mental illness, substance abuse, and crisis intervention.

Lindsay De Luna, LCSW
UCHealth Behavioral Health Clinical Co-Responder | noco.coresponse@uchealth.org
Lindsay joined to co-response team in January 2022. Lindsay holds a bachelor’s degree from Idaho State University and a Master of Social Work from University of Denver. She is credentialed as a Licensed Clinical Social Worker (LCSW). She has worked in several different hospitals as well as an inpatient behavioral health facility, primarily working with individuals experiencing a mental health crisis or dealing with substance use issues.

Cora Jessup, LCSW
UCHealth Behavioral Health Clinical Co-Responder | noco.coresponse@uchealth.org
Cora holds a Bachelor's in Social Work from Azusa Pacific University and a Master’s in Social Work from the University of Washington. She is currently credentialed as a licensed clinical social worker. Cora has worked across a wide spread of locations including LA, San Diego and Seattle in a variety of capacities including community mental health, hospice, inpatient behavioral health and community organizing. She started in co-response with the Greeley Police Department in early 2020 and was most recently on the Crisis Intervention Response Team (CIRT) with the Boulder Police Department. Her clinical specialties include complex trauma, crisis intervention, and grief/loss.

Officer Meagan Robinson
MHRT Officer | mhrt@fcgov.com
Officer Robinson has been with FCPS since 2015 and is Crisis Intervention Teams (CIT) Certified. She served on patrol and the Neighborhood Engagement Team (NET) before joining the Mental Health Response Team in 2022. Officer Robinson is looking forward to continuing and growing collaborative community partnerships. Her goal is to provide the best resources available to community members and offer appropriate long term support and care. She believes that having open communication, discussions and education allows for the community to take care of each other.

Officer Joe Schilz
MHRT Officer | mhrt@fcgov.com
Officer Joe Schilz has been with Fort Collins Police since 2019 and is a member of the department’s Peer Support Team. Joe is a certified CIT (Crisis Intervention Team) Coach and assists with training officers attending a CIT course. Joe is passionate about building relationships with community members and helping them in their time of need. Prior to becoming a police officer, Joe served in the U.S. Army as an Infantryman, and deployed to Baghdad and Baqubah, Iraq. Joe has earned an associate’s degree in Criminal Justice.

Officer Cory Kiper
MHRT Officer | mhrt@fcgov.com
Officer Cory Kiper has been a police officer since 2013. He began his police career with the Larimer County Sheriff’s office in 2013 and transitioned to Fort Collins Police Services in 2020. Before embarking on his career in policing, Cory proudly served in the United States Army, undertaking deployments to multiple locations in both Iraq and Afghanistan. Cory holds a bachelor’s degree in Criminology and Law Enforcement Administration. Cory is a Crisis Intervention Teams (CIT) coach. For over 12 years, Cory has been an active volunteer with various veteran organizations, passionately addressing critical issues such as Post-Traumatic Stress Disorder (PTSD) and veteran suicide. Cory is committed to serving the citizens of Fort Collins through a focus on community need and collaboration.

Sgt. Andrew Leslie
MHRT Supervisor | aleslie@fcgov.com
Sgt. Andrew Leslie is the Mental Health Co-Responder Sergeant. This role was added to the team in January 2022. Prior to his selection, Andrew was a patrol sergeant responsible for supervising a shift of officers covering a variety of calls for the City of Fort Collins. In this role, Andrew worked closely with members of MHRT to help streamline their processes and provided support and direction in the implementation of MHRT goals and objectives. One of Andrew’s strengths is building relationships, which he's worked to demonstrate in all of his professional and personal endeavors. Andrew truly believes there is nothing that can’t be accomplished when clearly-defined goals and responsibilities are implemented in a collaborative environment.

Rob Seals, Ph.D.
FCPS Police Psychologist - Coordinator
(970) 416-2958
Dr. Rob Seals is the 3rd on-staff Police Psychologist in the 30-year history of FCPS’ in-house mental health program. Dr. Seals is a USAF Veteran and Lieutenant Colonel in the USAF Reserves where he has provided mentorship to a team of behavioral health officers including psychologists, psychiatrists, nurse practitioners, clinical social workers, and mental health technicians. He offers confidential counseling to all staff and their families, provides crisis intervention services, coordinates the department’s peer support team, trains all new officers and dispatchers, and provides ongoing training for staff.

Lt. Dan Murphy
FCPS Special Operations Division
(970) 416-2660 | dmurphy@fcgov.com
Lieutenant Dan Murphy has been a police officer since 1984 and a supervisor since 1996. He has been assigned to supervisory positions in Patrol Operations, a County Drug Task Force, and the Criminal Impact/Fugitive Unit. He was assigned to SWAT Operations as the SWAT Sergeant full-time for 10.5 years. He has been the SWAT Commander since 2016, has been a SWAT Team Leader since 1995, and has been a SWAT officer since 1991. His lieutenant assignments have included the Professional Standards Unit, Patrol Watch Commander, and most recently, the Special Operations Commander of the SWAT team, the K-9 Unit, Bomb Team liaison and the Supervisor of the Co-Responder Mental Health Team. Lt. Murphy believes in and supports an agency-wide philosophy of de-escalation and solid tactical decision-making that saves lives.

